Some 1.3 billion of these people are pushed deeper into poverty or extreme poverty by the financially devastating costs of health care.
Overall, there has been little progress in recent years in efforts to ensure health insurance for every one of the world’s eight billion people, according to the WHO, but the organizations are determined to make health care accessible to a larger proportion of the population.
The World Bank recently announced a new goal: to help countries provide affordable health care to 1.5 billion people by 2030. World Bank President Ajay Banga said in a statement: “Providing lifelong basic health care is critical for development. This goal cannot be achieved alone. It requires partners, a coalition of public and private sectors working together to expand access to health services.”
Here are three initiatives aimed at expanding access to health care.
Artificial intelligence can tackle healthcare challenges
A significant shortage of health workers is a major factor limiting access to health care. The WHO estimates that there will be a deficit of 10 million health workers by 2030, mainly in low- and middle-income countries.
Research by the World Economic Forum has identified use cases for generative artificial intelligence (AI) that could partially overcome the challenges associated with the shortage of medical personnel.
The study finds that generative AI could increase the productivity of healthcare workers, allowing them to get more done with the same number of employees. As an example, the white paper states: “AI models can create images and text that are human-like enough to automate many of today’s manual tasks – from transcribing doctor visits and composing emails to summarizing clinical trials and sharing general health information.”
The study also shows how generative AI can accelerate the analysis of unstructured data sets to help healthcare professionals gain more accurate insights. AI-powered chatbots could also be used to “have more intuitive, human-like conversations with patients and caregivers that can help inform treatment decisions and prompt action.”
Another significant improvement that AI will bring is greater engagement with patients and healthcare services.

Deeper engagement could include early interventions to educate people about healthy lifestyles and disease prevention. When patients enter a healthcare facility, AI could provide a triage service to guide them to diagnosis or treatment. Another area where AI has potential is monitoring side effects and adherence to treatment programs.
Closing the gender gap in healthcare
More equitable treatment of women’s health issues could dramatically improve the lives of over 3.9 billion people, according to a groundbreaking report, “Closing Women’s Health Gap: A $1 Trillion Opportunity to Improve Lives and Economies,” which finds that more effective health care for women would reduce the time they spend in poor health by two-thirds.
The release of the report at the 2024 Davos Congress coincided with the launch of the Global Alliance for Women’s Health, which aims to promote and prioritize women’s health. Although women live longer, they also experience illness more often, often during the most productive period of their lives.
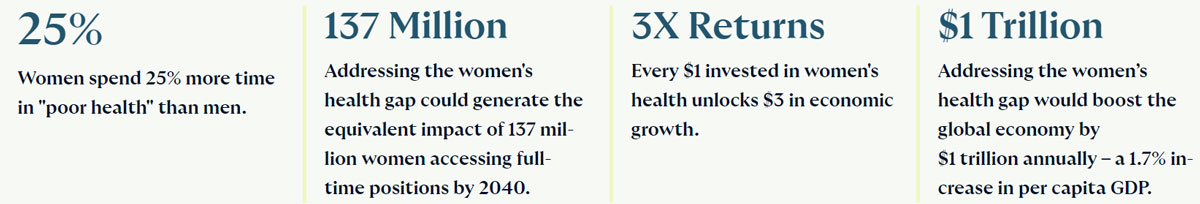
There is a significant lack of data on women’s biology and there is not enough research on women’s health issues.
This deficit affects both women-specific and cross-gender diseases, but is expressed to varying degrees among women. For example, less than two percent of medical research funding goes to the areas of pregnancy, childbirth and women’s reproductive health.
Combating degenerative diseases
Access to treatments and medications for disabling disorders and diseases of the nervous system such as Parkinson’s, Alzheimer’s, epilepsy, multiple sclerosis and dementia is limited – and in some cases completely impossible.
These diseases are the leading cause of disability worldwide, according to a WHO report. The report highlights the inconsistency in care and drug availability, saying: “Although effective medicines exist that can prevent, treat and/or alleviate symptoms and significantly improve the quality of life of people with neurological disorders, the persistent lack of access contributes significantly to the treatment gap.”
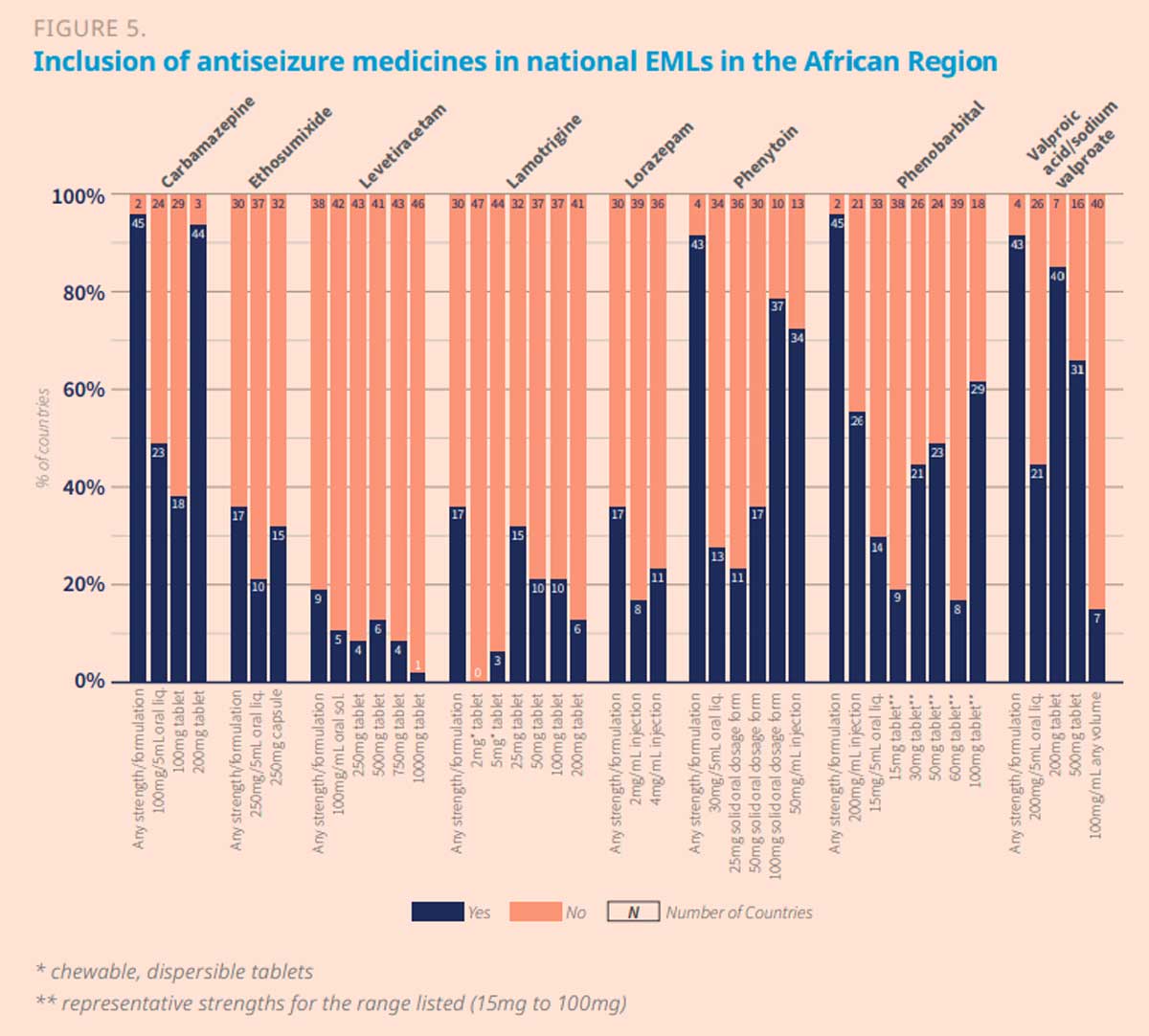
Closing this treatment gap requires, on the one hand, educational work to overcome the stigma associated with neurological diseases and, on the other hand, the classification of medicines for these conditions as essential medicines in all countries.
In a blog post, Shyam Bishen, director of the Center for Health and Healthcare at the World Economic Forum, writes: “For example, drugs for Parkinson’s and epilepsy are not widely included in essential medicines lists in African countries, nor are specific formulations of some drugs such as antiepileptics for children. This may make them less likely to be prioritized for procurement and reimbursement.”
Limited registration of key medicines for neurological diseases represents a significant barrier to access, as unregistered medicines cannot be legally sold or distributed. WHO recognizes this challenge and is working with various countries to optimize their registration processes. Improving registration procedures is critical to improve procurement opportunities and increase overall health system capacity.
Collaboration is critical to addressing a wide range of health challenges. With joint efforts and a willingness to share knowledge and best practices among stakeholders, we can develop and scale up solutions for more equitable health systems.

